In this section we will look at some topics related to the health and wellbeing of our senior citizens. Each topic is written by expert geriatricians based on real life experiences.
Polypharmacy in Older Adults

Polypharmacy is defined as the regular intake of at least five medications. It is very common in older adults. There are several risk factors that can lead to polypharmacy; patient related factors include having multiple medical conditions managed by multiple subspecialist physicians, having chronic mental health conditions, and residing in a long-term care facility. One must reduce the intake of drugs by asking the doctor the necessity of a particular drug. In the book by Dr. Prasun Chatterjee (Health and well being in late life, chapter: Challenges of Multimorbidity and Polypharmacy in Older Adults), he has explained the issue of polypharmacy by the case of Kamala Sarkar, who was actually a patient of his. Mrs. Kamala had visited several doctors with her extensive list of complaints. She has a prescription of 19 medicines (polypharmacy) along with her. Her medicine included three types of antihypertensive; three groups of drugs for lowering blood sugar levels; three medications for managing arthritis; one multivitamin; one medicine each for calcium, vitamin D, Vitamin B12 and depression along with sleeping pills and three medicines for coronary heart diseases. She was on consultation with many doctors and each healthcare provider has provided organ specific medicines based on history of complaints. Unfortunately, clinical practice is restricted to organ specific and disease specific guidelines. Patient like Mrs. Kamala, suffering from multimorbidity, would visit multiple specialists for separate problems, ending up with multiple drugs, even if the specialist follows evidence based medicine. Based on this example, one should inform the doctor about all the medicine intake and ask the doctor about any kind of reaction of the medicines which are being continued.
Consequences of polypharmacy:
There are many negatively associated consequences with polypharmacy. Specifically, the burden of taking multiple medicines has been associated with an increased risk of adverse drug events (ADEs), drug interactions, medication non-adherence, reduced functional capacity and multiple geriatric syndromes.
- Increased Healthcare Costs: polypharmacy contributes to health care costs to both the patients and the healthcare system. A retrospective cohort study found that polypharmacy was associated with an increased risk of taking a potentially inappropriate medication and an increased risk of outpatient visits, and hospitalization with an approximate 30% increase in medical costs.
- Adverse Drug Events: It has been reported that 35% of the outpatients and 40% of the hospitalized elderly experience ADE. As one might expect, common drug classes associated with ADEs include anticoagulants, NSAIDs, cardiovascular medications, diuretics, antibiotics, and hypoglycemic medications.
- Drug-Interaction: older adults with polypharmacy are predisposed to drug-interactions. Drug-drug interactions are a frequent cause of preventable ADEs and medication-related hospitalizations. Thus practitioners should keep the possibility of a drug-drug interaction in mind when prescribing any new medications.
- Medication Non-adherence: It is linked to complicated medication regimens and polypharmacy in older adults. Medication non-adherence is associated with potential disease progression, treatment failure, hospitalization, and ADEs, all of which could be life-threatening.
- Functional status: Polypharmacy has been associated with functional decline in older patients. In a prospective study of community-dwelling older adults, increased prescription medication use was associated with diminished ability to perform instrumental activities of daily living (IADLs) and decreased physical functioning. . In patients who have reported falling in the past year, higher medication use was found to be associated with functional decline. Prescribers should be aware of the risk of functional decline in patients taking multiple medications.
- Cognitive Impairment: Cognitive impairment, seen with both delirium and dementia, has been associated with polypharmacy. A study in hospitalized older adults reported that the number of medications was a risk factor for delirium.
- Falls: Falls are associated with increased morbidity and mortality in older adults and may be precipitated by certain medications. A study comparing patients who have not fallen compared to those who have fallen once and those multiple times, reported that the number of medications was associated with an increased risk of falls. Given the serious consequences of falls in older adults, caution should be used in prescribing new medications to those who are at risk of falling.
- Urinary Incontinence: It is yet another problem that is associated with the intake of multiple medicines. Many medications are known to exacerbate urinary incontinence, so a medication review should be performed to evaluate both the number of medications as well as the specific types of medications a patient is taking.
- Nutrition: Polypharmacy has also been reported to affect a patient’s nutritional status. A prospective cohort study found that 50% of those taking 10 or more medications were found to be malnourished or at risk of malnourishment .
ACTIVE AGING

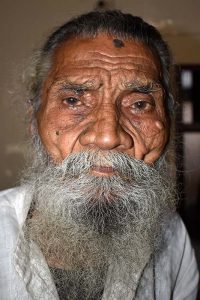
I want to go to park for a walk, but my leg muscles are not strong enough to take even a few steady steps. I am weak, shaky and slow. I am not depressed but I am not happy either. The doctor assures me that my heart, lungs and organs are totally fine. I know I should eat a proper diet and do exercises, but I do not feel motivated to do anything except to just escape this life. The only thing that is remaining in me is my beautiful mind that urges me each day to love all and pray for all. I often wonder whether these are the features of a fast decaying mind or body. Or these are just the perceptions and emotions of a frail person.
The above are the words of a 87 years old person, a retired banker. He wrote a letter to Dr. Prasun Chatterjee, Department of Geriatric Medicine, AIIMS, New Delhi, expressing his thoughts and emotions. Ageing is probably and individualistic and unique experience, which happens to occur through various biological events throughout the person’s life.
What is active aging? Active aging is the process of optimizing opportunities for health, participation and security in older adults in order to enhance quality of life as people age. Active aging applies to both individuals and population groups. It allows people to realize their potential for physical, social, and mental well being throughout the life course and to participate in society according to their needs, desires and capacities, while providing them with adequate protection, security and care when they require assistance. The active ageing model as presented by the World Health Organization (WHO) encompasses six groups of determinants, each one including several features:
- Availability and use of health and social services
- Behavioral determinants
- Personal determinants
- Physical environment
- Social determinants
- Economic determinants
Health refers to physical, mental and social well being as expressed in WHO definition of health. Thus, in an active aging framework, policies and programs that promotes mental health and social connections are as important as those that improve physical health status.
WHO defines healthy ageing as “the process of developing and maintaining the functional ability that enables wellbeing in older age.” Functional ability is about having the capabilities that enable all people to be and do what they have reason to value. This includes a person’s ability to:
- meet their basic needs;
- learn, grow and make decisions;
- be mobile;
- build and maintain relationships; and
- Contribute to society.
Functional ability consists of the intrinsic capacity of the individual, relevant environmental characteristics and the interaction between them.
Intrinsic capacity comprises all the mental and physical capacities that a person can draw on and includes their ability to walk, think, see, hear and remember. The level of intrinsic capacity is influenced by several factors such as the presence of diseases, injuries and age-related changes.
Environments include the home, community and broader society, and all the factors within them such as the built environment, people and their relationships, attitudes and values, health and social policies, the systems that support them and the services that they implement. Being able to live in environments that support and maintain one’s intrinsic capacity and functional ability is key to healthy ageing.
https://extranet.who.int/agefriendlyworld/wp-content/uploads/2014/06/WHO-Active-Ageing-Framework.pdf
https://www.frontiersin.org/articles/10.3389/fmed.2017.00181/full
STROKE
Stroke is a global health problem and is a leading cause of adult disability. Driven by increasing size and aging of the populations, and escalating prevalence of risk factors such as hypertension, tobacco use, unhealthy diet, physical inactivity and obesity stroke is becoming a major cause of premature death and disability in developing countries. This prompted the World Health Organization (WHO) to launch the Global Stroke Initiative aimed to generate population based data on burden of stroke and to use such data to evolve strategies for prevention and management. Recent research suggests, however, that cardiovascular risk may not be limited to specific negative mood states such as depression, but extends to psychosocial distress, a broader concept defined as the tendency to experience stress, negative events, and more generally a negative outlook on life. Less is known about the effect of psychosocial distress on risk for stroke morbidity and mortality.
In 2015, a patient with prognosis of Stroke was admitted to AIIMS, Delhi under the supervision of Dr. Prasun Chatterjee in Department of Geriatric Medicine. During the examination the patient had right-sided complete weakness and was only responding to painful stimulus but was restless within. By the same day evening, her consciousness improved but was not able to speak. After examining the CT scan of the brain it was observed as the occlusion of blood vessels in the left sided brain, which supply blood to most important part of the brain- Broca’s aphasia, which controls speech. Ageing is the most common and irreversible risk factor for brain stroke. The patients’ daughter kept questioning the doctor about her mother prognosis to which Dr. Prasun Chatterjee made her explain the e theory of life-course approach; vascular phenomenon like cardiovascular diseases and stroke may have long natural history with accumulation of risk beginning in early life and continuing through childhood into adolescence and adulthood. The life-course overview considers physical as well as social perils and the ensuing behavioral, biological and psychosocial systems, which act across all levels of the lifespan to affect disease risk in the later years of life. The stages of lifespan include gestation, infancy, childhood, adolescence, young adulthood and midlife. Stroke in the very elderly may present atypically, especially when there is synergism of multimorbidity, geriatric syndrome and age-related delayed response of the body. In this case, her pre-morbid status was not optimal, with minimal mobility, and the motivation to walk was almost none.
Risk factors and the incidence of stroke peak in subjects aged 75 years or older. Patients with the highest risk benefit most from the effective risk reduction therapy. Control of hypertension, resolution of dyslipidemia, management of diabetes mellitus, anticoagulation for AF, promotion of exercise and healthy diet, and cessation of cigarette smoking are obligatory.
For management and other related information got through the links.
https://www.ahajournals.org/doi/full/10.1161/STROKEAHA.112.679159
https://bmcneurol.biomedcentral.com/articles/10.1186/s12883-021-02353-y
https://www.ahajournals.org/doi/pdf/10.1161/STROKEAHA.108.531293
https://link.springer.com/chapter/10.1007/978-981-13-8938-2_7
BONE HEALTH IN OLDER ADULTS

Age and bones have a love-hate relationship. When we are young our bones are in better shape and functioning, but as we start to age, bone health starts getting affected. This is the reason, why each and every one of us should be informed about the bone health. Osteoporosis is a major public health problem worldwide. World Health Organization (WHO) puts this disease second along with the cardiovascular diseases at the top, on the list of serious global healthcare problems. Studies have reported that Asian women have higher predisposition for the osteoporosis than their Caucasian counterparts. About 1 in 3 women over the age of 30 years of age experience fractures related to osteoporosis. The attainment of peak bone mass in adolescent years and the rate of bone loss during postmenopausal years are some of the major factors contributing to bone health in older women. The rate of bone loss accelerates during the early postmenopausal years. The accelerated bone loss in the post menopausal osteoporosis is a result of decline estrogen concentrations. According to WHO, it is an under-recognized public health concern that needs immediate attention. The lack of knowledge and awareness about this crippling disease has translated into a significant human and economic burden on India. While osteoporosis has been known to commonly affect menopausal women, improper dietary habits and an increasingly indoor lifestyle are now putting the relatively younger generation at risk. The lack of awareness about the disease and specific osteoporosis guidelines further raise concerns about its growing trend in the country.
Take-home messages for optimum bone health in the elderly one need to select food rich in calcium like low-fat milk, low-fat dairy products like yogurt, homemade curd, paneer, custard, low sugar soft niger seed chikki/foxnut (makhana) kheer, calcium-enriched soymilk, kidney beans, cow peas, moth beans, lentils, whole red gram, whole Bengal gram, whole greengram, whole black gram, and whole horse gram, almonds or its milk, gingelly seeds (black/brown/white), dried figs, vegetable leaves like amaranth/ bathua/ fenugreek/ colocasia/mustard/ raddish/ drumstick/ knol-khol, spices like cloves, cardamom, cumin seeds, coriander seeds and sardines as a good choice .Instead of staple rice and wheat replace some days with millets like ragi, amaranth seeds (Rajgira) which are calcium-rich. For vitamin D fortified milk and its sources, cereals (wheat flour/rice), edible vegetable oil; salmon, sardines, mackerel, egg, liver along with exposure to sunlight for at least 45 minutes between 10.00 am to 02.00pm in India should be followed. Weight-bearing exercise on a chair with correct posture and balance under expert supervision should be initiated with warm-up workout and relaxation along with the practice of walking and gardening has to be taken care of for good bone health with ageing.